For years, families were told the same story: plaques build up, memory fades, nothing much to be done. Now a wave of lab data and hospital scans is flipping that old script, shocking even seasoned researchers. If the new picture holds, the focus of Alzheimer’s care could shift from chasing plaques to protecting the brain’s delicate gatekeepers.
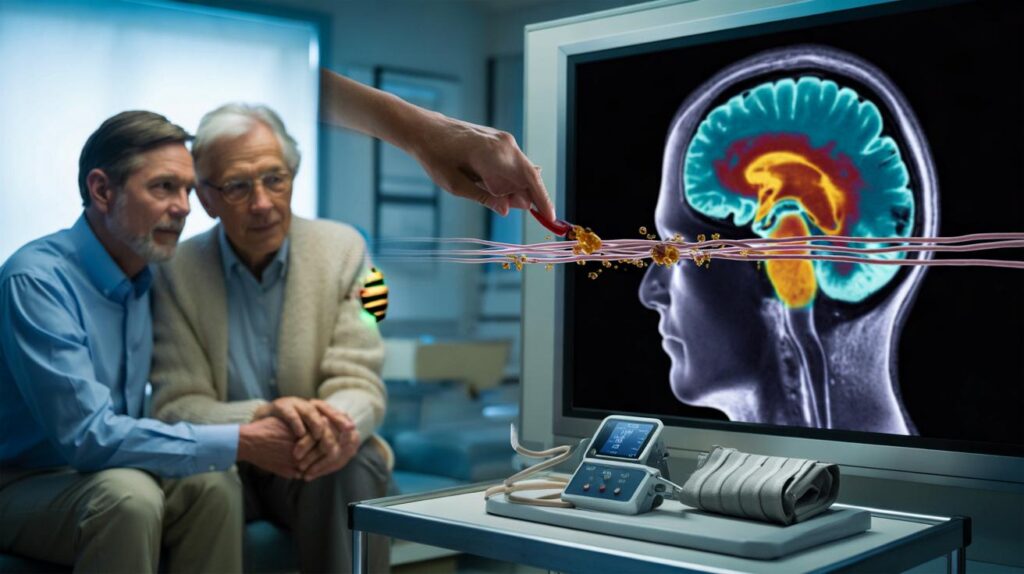
The lift doors open onto a quiet memory clinic, and a kettle ticks in the staff kitchen. A consultant straightens her ID badge as an older couple shuffle in, hands linked, the way people do when they’re holding each other up as well as saying hello. I watch the screen glow with a fresh brain scan while the researcher murmurs about “leaks” showing up in places where leaks should never be. It looks like rain seeping through a roof that was meant to be watertight.
Outside, the city rushes on, but in this room a new idea hangs in the air. The brain’s defences are not a footnote — they might be the story. Something had shifted.
The discovery rewriting Alzheimer’s
Here’s the twist: scientists are seeing early breakdowns in the blood–brain barrier, the paper-thin lining that keeps the brain’s chemistry stable. Tiny breaches let blood proteins trickle in, lighting up the immune system like a false fire alarm. Microglia swarm, inflammation crackles, and the damage spreads in places tied to memory and navigation.
On dynamic MRI scans, contrast dye seeps into the hippocampus in people with mild cognitive symptoms, years before a formal diagnosis. In mouse labs, when fibrinogen — a clotting protein — slips across the barrier, neurons lose their spines and circuits misfire. We’ve all had that moment when a name slips and panic pricks the neck. Imagine that feeling anchored not just to plaques, but to a leaky gate and an overzealous clean-up crew.
What stunned researchers wasn’t only the leak — it was the cascade. If barrier cells falter, amyloid and tau may become accelerants rather than the original spark. That would explain why drugs that only sweep plaques have helped some people a little, and not others as much. **This flips the Alzheimer’s story on its head.** The target shifts upstream, towards vascular health, barrier repair, and calming misfiring immunity.
What this means for treatment, today
Think of the brain’s defence line as a living tissue you can nurture. Sleep is not a luxury; it’s overnight maintenance for the brain’s waste-clearing system. Aim for a steady bedtime, cool and dark room, morning daylight on your face, and a quiet hour before lights-out with no bright screens.
Walk after meals to tame blood sugar swings, which stress small vessels. Keep blood pressure in a healthy range through movement, medication if prescribed, and salt awareness. If your partner has noticed loud snoring or pauses in breathing, push for a sleep apnoea check — oxygen dips batter the barrier over time. Soyons honnêtes : personne ne fait vraiment ça tous les jours.
There’s also a new angle for clinics: the combined approach. Anti-amyloid antibodies look different when paired with barrier-friendly care, better blood pressure control, or ultrasound programmes designed to open and reseal the barrier in a controlled way. **The real revolution may be timing.**
One NHS researcher put it plainly:
“If you protect the barrier and quiet the immune overreaction, the rest of our tools start to work harder for the brain. It’s like fixing the roof before you repaint the walls.”
Here’s a quick checklist to take to your GP or memory clinic:
- Ask about blood pressure targets suited to brain health, not just the heart.
- Screen for sleep apnoea and hearing loss, both linked to faster decline.
- Discuss blood biomarkers such as p‑tau217 as they roll out in pilots.
- Review medications for any that disturb sleep, blood pressure, or cognition.
- Plan a 12-week routine: walking, strength work, and a Mediterranean-style plate.
A new map of Alzheimer’s
When you start from the barrier, lots of puzzles line up. Silent mini-strokes, midlife hypertension, diabetes, gum disease, long-run noise or air pollution — all the boring villains of modern life — stress the same endothelial cells that guard our neurons. Those cells and their astrocyte partners hug the brain’s capillaries, and when they falter, chemistry sloshes where it should stay still.
That may be why some people with hefty plaque loads keep thinking clearly, and some don’t. Resilience isn’t a magic gene; it looks like a web of protections. Diets rich in colourful plants and healthy fats feed vessel walls. Exercise sends shear stress that tells arteries to behave. Treating hearing loss lowers cognitive load and social withdrawal. **Small habits, big brain pay-off.**
Zoom out from the lab bench, and you see a more human picture. The conversation in clinics moves from “wait and see” to “let’s stabilise the ground you’re standing on”. Blood tests that flag brain proteins in the bloodstream are stepping out of trials and into pilot services. It means earlier choices, better triage, and less guesswork for families trying to plan their lives.
The next question is a brave one: how early is early enough? If barrier leaks can show up before memory tests sputter, should we be screening people in their 50s with vascular risks? Imagine being told you have a window — not a sentence — and that treatment is a bundle, not a single shot. That changes the tone of the entire journey.
Researchers are testing cocktails: drugs that calm microglia without flattening them, compounds that stabilise barrier junctions, antibodies that mop up misfolded proteins, ultrasound to usher medicine in and then step back. It’s not headline magic. It’s steady, joined-up repair. Let’s be honest: nobody does that every day, but teams can design care to make it easier to live.
Clinical trials in the UK, EU, and US are already weaving these ideas together. Some use focused ultrasound and microbubbles to briefly open the barrier in pinpoint areas, then combine with targeted medicine and rest to let it reseal. Others track blood pressure variability and sleep depth as co‑primary outcomes, not just side notes. That’s a cultural shift as much as a scientific one.
Families care about the ordinary moments: making tea, finding keys, telling the right story at the right table. A treatment era that guards the brain’s border could protect those tiny freedoms, not just slow a score on a graph. That’s the promise humming through the scanners and the lab benches tonight.
All of this comes with caveats. Early studies don’t always scale, and biology loves to surprise us once we move from mice to messy human lives. Yet the direction of travel feels different this time. We’re moving from sweeping smoke to turning off the gas.
What should you do with this? Share it with the person who handles prescriptions in your family. Ask one practical question on your next GP visit. Try one small change you might actually keep. It’s not a cure. It might be something better — a way to steady the ground under our feet while the science sprints ahead.
| Key points | Details | Interest for reader |
|---|---|---|
| Barrier-first model | Early leaks in the blood–brain barrier appear before major symptoms and drive inflammation | Explains mixed results of plaque-only drugs and points to upstream targets |
| Combo therapies | Pairing antibodies with barrier repair, sleep care, and vascular control shows promise | Realistic pathways to better outcomes without waiting for a single miracle |
| Action today | Sleep routines, walking after meals, BP checks, apnoea screening, hearing support | Concrete steps families can discuss with clinicians right now |
FAQ :
- What exactly is the new discovery?Multiple studies suggest that small leaks in the blood–brain barrier can precede and amplify Alzheimer’s changes by triggering chronic inflammation.
- Does this mean plaques and tangles don’t matter?They still matter, but they may be downstream. Treating the barrier and immune response could make anti‑amyloid and anti‑tau drugs work better.
- How might treatment change?Expect combined care: vascular risk control, sleep treatments, barrier‑stabilising approaches, and targeted drugs delivered at earlier stages.
- Can I test for this now?Advanced MRI can show barrier leaks in research settings. Blood tests like p‑tau217 are moving into pilots and may guide earlier decisions.
- What can I do this week?Prioritise consistent sleep, a daily walk, blood pressure checks, hearing support, and a conversation with your GP about risks and screening.


Game‑changer? Show me human outcomes beyond pretty MRI pics, please. Cautiosly hopeful.